Analgesia for normal labor and delivery
Introduction:
The experience of child birth ranges from agony to ecstasy. One of the most thrilling and gratifying experience in mother life will be the birth of her child. Labour pain rank among the most intense pain, as recorded on McGill pain questionnaire 1 and it is typically worse than a toothache, back pain, & pain associated with a deep laceration. The development in labour analgesia also signifies the change in thinking and attitude to the relief of pain in labour. The more concern are now of mother & baby safety.
Effects of labour pain on mother:
This intense nature of labour pain causes release of catecholamines, all the stress har-mones,and sympathetic stimulation. This causes maternal exhaustion, maternal hyperventilation, increased oxygen consumption and hypoxic episodes. During labour, cardiac output increases by 10-25% and blood pressure by 5-20% with each contraction.
Factors affecting pain perception in labor:
Mental preparation, Family support, Medical support, Cultural expectations, Underlying mental status, Parity, Size and presentation of the fetus, Maternal pelvic anatomy, Duration of labor, Medications.
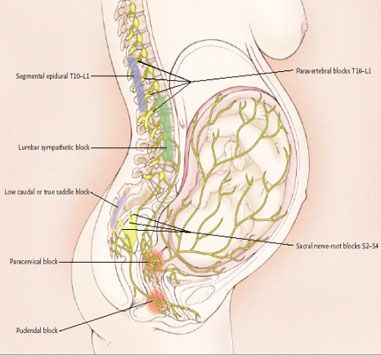
Pain Pathways in Labor and Delivery 2:
Pain of labour arises primarily from nociceptor in uterine and perinial structures. Afferent nerve fibers transmitting pain sensation during first stage of labour from cervix & uterus travel with sympathetic fibers to enter neuraxia at thoracic 10th, 11th, 12th & 1st lumbar spinal segment. In late first stage & second stage of labour, pain impulses increasingly originate from pain sensitive areas in perineum & travels via pudendal nerve to enter 2nd, 3rd, & 4th sacral segments. The pain at different stages differs in intensity. The latent phase from 0 to 3 cm of cervical dilatation, the pain is minimal so require no analgesia. During active stage from 3 cm to full dilatation & become more intense, at this stage epidural &spinal analgesia can be given. During second stage from cervical dilatation to child birth pain intensity is maximal and there after it decreases gradually.

The Ideal Labor Analgesic technique:
Should have Good pain relief, No autonomic block (no hypotension),No adverse maternal or neonatal effects, No motor block, No effect on labor and delivery, No increase in C/S rate, No increase in forceps/vacuum delivery, Patient can ambulate, Economical: cost effective.
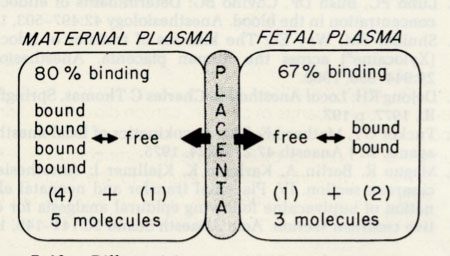
Factor affecting Placental Transfer of Drugs:
Lipid solubility, Molecular size, Total dose of drug, Concentration gradient, Maternal metabolism and excretion, Degree of ionization, pKa of drug, maternal and fetal pH, Protein binding – mother and fetus, Uterine blood flow, Time for equilibrium to occur.
Only free drug i.e unbound drug is transferred across placenta, more the protein bound drug less will be transfer.

Analgesic Technique used for vaginal delivery:
Is divided into two groups, Pharmacological and Nonpharmacological.
➤ Pharmacological
1) Systemic Narcotics, 2) Regional analgesics. 3) Tranquilizers / Hypnotics 4) Inhalation analgesics.
➤ Nonpharmacological
1) Acupuncture 2) Sterile water block 3) Transcutaneous electric Nerve stimulation 4) Psycho analgesic Techniques
Nonpharmacological 3:
Acupuncture: This is traditional form of Chinese medicine involving the insertion of needles at selected points to get desired effects. The results were conflicting and found to be ineffective in almost 80% of cases.
Sterile water block: Intracutaneous injections of sterile water in the skin over the sacrum have been shown to relive first stage back pain. Using a 25-gauge needle, four 0.1 to0.15 ml papules of non preserved sterile water are injected into the intracutaneous skin of sacrum during contraction. These injections produces osmotic stimulation from salt free water and distention pain incutaneous layers, thus stimulating skin nociceptor and inhibiting pain transmission to the dorsal horn.
Transcutaneous electric nerve stimulation: This method is thought to work by the Gate control theory – activation of fast conduction Ab fibers by TENS close the gate for transmission of slow conducting Ad and C fibers which transmit pain impulses.
Psycho prophylaxis: In 1958 Lamaze reported success of Psycho prophylaxis achieving analgesia during labour. In this pain relief was achieved by creating conditional reflexes in mother and educating her about the process of natural birth but many other reported incomplete analgesia.
Systemic Opioids in Labor
One of the convention methods of giving labour analgesia is systemic opioids. Morphine was first Opioids used for a labour analgesia
The advantages of Systemic Opioids in labour
Systemic opoids are easy to administer, they are Inexpensive, They require no special needle which are require for regional analgesia, They avoids the complication of Regional Block like Hypotension, High Sensory Block, Post Dural Puncture Headache and they does not require any skilled person
Disadvantages of Systemic Opiods
Opioids can easily crosses placenta, Most of the cases have inadequate pain relief, GI disturbances such as nausea, vomiting, gastric stasis, Causes maternal sedation, Also effects on fetal heart rate i.e. loss of beat to beat variability and sinusoidal rhythm. Dose related maternal and neonatal depression, Some times systemic Opioids causes newborn neurobehavioral depression.
The various systemic Opioids which can be given during labour are traditional one like morphine, mepridine and Newer like fentanyl, Alfentanyl, Ramifentanyl, But fentanyl, is widely used because of shorter duration of action and minimal newborn effect.
Potential Fetal/Neonatal Effects of Maternal Sedation due to systemic Opioids:
Low 1 and 5 min Apgar scores, Respiratory acidosis, Naloxone, ventilatory assistance may be needed, Neurobehavioral depression – dose dependent, prolonged observation in NICU occasionally needed.
Neonatal Neurobehavioral Effects of Maternal Systemic Medication:
Transient, global depression of behavior related to presence and quantity of drug in new-born, Most effects gone by 3rd day; all by 10 days, Important and very difficult to differentiate from sinister causes like Down’s syndromes, congenital CNS abnormalities.
Inhalation Analgesia for Vaginal Delivery 5 :
N2O:O2 in 50:50 mixtures, this mixture is called as entonox.
Advantages: (1) self administered (2) taken on demand delivery that means at the onset of uterine contraction, patient starts inhaling the mixture,& by the time when uterine contraction is maximum, patient is pain free & at the end of contraction patient should removes mask. Gives good analgesic effect with adequate level of consciousness. (3) Causes minimal neonatal depression.
Disadvantage: (1) Decreased uterine contractility (except N2O), (2) Risk of unconsciousness and aspiration, (4) Difficulties with scavenging in labor rooms.
Local techniques for labour and delivary:
1) Local infiltration,2) Pudendal block, 3) Paracervical block, 4) Paravertebral (lumbar sympthetic block).


Paracervival Block:
It is relatively simple block to perfom, provides pain relief for the first stage of labour, and offers no pain relief for second stage. Local anesthetic is injected submucosally into the fornix of the vagina lateral to the cervix and uterus. Its use in obstetrics has been limited by profound fetal bradycardia, systemic local anesthetic toxicity, postpartum neuropathy and infection. Fetal bradycardia is due to decreased uterine blood flow and high fetal blood levels of local anesthetic.
Regional Analgesia for Labor:
This technique is becoming popular now, these technique are 1) Lumbar epidural 2) Caudal epidural 3) Spinal 4) combined spinal epidural.
Epidural analgesic technique 6:
With all aseptic precaution epidural space is identified at L3-L4 space with loss of resis-tance technique using Tuohy needle and catheter is introduced 2 to 3cm inside epidural space. Position of catheter is confirmed by negative aspiration of blood or CSF.Ones the labour is well established with strong contraction lasting about 1 min each and occurring at 3 min interval 1st dose is given and it is supplemented with intermittent top up or continuous infusion per hourly. 0.1% Bupivacaine + fentanyl 1- 2µg/ml.10ml is used as a first dose for ambulatory or walking epidural regimen. Opioids cause inadequate analgesia if used alone. These Synergize with local anesthetics which speeds the onset of analgesia and which ultimately improve quality of analgesia and permit use of dilute LA solutions.
Maintenance of analgesia: Repeat bolus dose with more dilute local anesthetic mixture using 0.0625 to 0.1% bupivacaine and 1-2µg/ml fentanyl 10 ml/hr.
Continuous Infusion Epidural 7:
A larger volume of a more dilute agent is more effective for labor analgesia than a small volume of higher concentration. Instrumental vaginal delivery rate is decreased by giving combine continuous epidural infusion of bupivacaine and fentanyl rather than giving only bupivacaine.
Patient controlled epidural analgesia during Labor4:
Analgesia is established by means of either spinal or epidural, the catheter is connected to the PCEA device, and then Patient can self administer the boluses of drug as required with a specific lockout period of 10 minutes. The advantages are, to reduce demands of staff on the labour floor, feeling of empowerment to patient, total amount of drug is reduced to provide same analgesia.
Walking Epidural: With low dose local anaesthetic and opioid combination in continous epidural analgesia, walking in labour with good pain relief is possible and is associated with greater degree of maternal satisfaction.
Walking in labour may have atleast three theoretical advantages.
- Gravity may effect the rate of cervical diliatation
- The movement of pelvis may encourage correct position of the fetal head.
- Being upright may decrease any tendency to aortocaval compression
Safe Ambulation with labour analgesia Prerequisites :
- No postural hypotension or symptoms
- No motor or Proprioception block
- Fetal monitoring ( Remote,cordless )
- Co-Operative and understading parturient
- Provision of suitable conditions
- Good epidural catheter fixation
- Disconnected IV line
- Safe floor without cables.
Combine spinal epidural analgesic technique 8:
CSE is usually performed at mid to low lumbar intervertebral space using needle through needle technique. Epidural space is identified with 16G epidural needle and then 25G spinal needle is inserted through epidural needle in to sub arachnid space. Proper placement is confirmed by free flow of CSF. Analgesia is achieved rapidly within 60 seconds using low dose Opioids and local anesthetic combination 2.5 ml 0.1% bupivacaine and 2µg/ml (5µg) fentanyl intrathecally. The epidural catheter is introduced and maintenance is achieved by intermittent bolus of 0.05% bupivacaine + 1µg/ml fentanyl 10ml, or continuous infusion of 0.05% bupivacaine + 1µg/ml fentanyl 10ml/hr.
Advantages of CSE (Opioids ± local anesthetic) for Labor Analgesia
There is Rapid onset of analgesia (the patient loves you immediately),CSE is ideal in late or rapidly progressing labor, it has Very low failure rate, uses of this technique causes less need for supplemental boluses. This causes minimal motor block, it has the benefit of allowing maternal ambulation, if desired & is offen refferred to as a walking epidural.
Complication of intrathecal Opioids or combined spinal epidural analgesia8:
Severe hypotension, respiratory depression, high sensory block, severe fetal bradycardia & infection. Other problems are technical failure i.e. needle two short, needle deviates from midline. Drug mixing errors, Post dural puncture headache, pruritus,& nausea & vomiting.
Strategies to Decrease Complications with CSE:
Decrease dose of Opioids by combining these Opioids with local anesthetic, Epinephrine, clonidine.
Current Recommendations for CSE:
Use lowest effective dose of Opioids, & if possible don’t repeat the dose. While giving CSE monitor BP, FHR, Respiration and SpO2.If local anesthetic mixture is hypobaric avoid prolong sitting position after block.
Advances in Modern Obstetric Analgesia:
➤ Technical Advances: USG guided localization of the epidural space used as visual aid/diagnostic tool or for teaching aid and Electrical stimulation by Tsui needle causes muscle twitch elicited with electrical stimulation during catheter insertion, indicate epidural needle localization.
➤ Technological Advances: Mobile pumps, PCEA/PCIV pumps, Elastomeric pumps, Epidural /spinal kits & catheters. These have leaded us to newer infusion regimes.
Provision of neuraxial analgesia early in labour has distinct advantages for maternal analgesia and satisfaction, with no negative impact on mode of delivery.
Fetal / Neonatal Effects of Regional Analgesia in Labor 9 :
Uterine perfusion maintained until profound hypotension & possible fetal compromise. Local Anesthetic toxicity is extremely rare. FHR changes like baseline variability, periodic decelerations. Apgar scores, acid-base status is unaffected. Neurobehavioral effects absent with current agents.
Fetal Bradycardia after Labor Analgesia :
Pain relief in mother causes decreased circulating epinephrine, this leads to increase in uterine tone or uterine hyper stimulation. This decreases uterine blood flow & causes fetal bradycardia.
Management of FHR Changes 10 :
Include maternal position change i.e. left lateral position and in supine position left uterine displasement, supplemental oxygen administration. For the treatment of uterine hyper stimulation inj. Terbutaline (1.25 mg to 2.5 mg sub cut) or nitroglycerine 0.4 mg to 0.8 mg in 2 puffs sublingual can be useful. Treatment of maternal hypotension by giving IV fluids in boluses or inj. Ephedrine.
References:
- Melzack R, Taenzer P, Feldman P, Kinch RA. Labour is still painful after prepared childbirth training Can Med Assoc J 1981:125:357-63..
- The Nature of pain of parturition. Clin obstel gynaecol 1975;2.5111.
- Simkin P. Reducing pain and enhancing progress in labour : a guide to Nonpharmacological method for maternity caregivers. Birth 1995;22:161-171.
- Mclntosh DG.Rayburn WF. Patient controlled analgesia in obstetics and gynecology. obstet gynaecol 1991; 78: 1129-35.
- Rosen M. Recent advances in pain relief in childbirth. I. Inhalational and systemic analgesia.Br J Anaesth 1971 :43: 837-48.
- Robinson JO, Rosen M, Evans JM,et al. Maternal opinion about analgesia for labour. A Controlled trial between epidural block and intramuscular pethidine combined with inhalation. Anesthesia 1980;35:1173-81.
- Gambling DR, YU P,cole c, et al. A Comparative study of patient controlled epidural analgesia and continuous infusion epidural analgesia during labour. Can J anesth 1988;35: 249-54.
- Hepner DL, GAISER RR, cheek T4,Gutsche BB. Comparison of combined spinal –epidural and low dose epidural analgesia in labour. Can J Anesth 2000:47:232-6.
- Palmer CM, maciulla JE,Cork RC et al. The incidence of fetal heart ratechanges after intrathecal fentanyl labour analgesia.
- Bell E. Nitroglycerin and uterine relaxation. Anesthesiology 1996;85:683