Mitral Stenosis [MS]
☛ Etiology – congenital / Acquired [adult ]
☛ Congenital MS is very rare .Associated with other anomalies as shave’s complex
☛ Acquired – Moss common is Rheumatic heart disease
☛ 25% rheumatic heart disease pure MS.
☛ 40% have MS with MR.
☛ 10% have pure MR.
Rare causes are
- Systemic lupus erhythmatosis.
- Rheumatoid arthritis.
- Amyloidosis.
- Hurlers and Hunter disease.
- Methysergide therapy.
Other conditions do not directly involve MV but may limit LV inflow are
- Cortriatriatum
- Large LA neoplasm
- Pulmonary vein obstruction
Anatomy
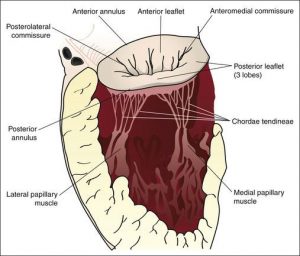
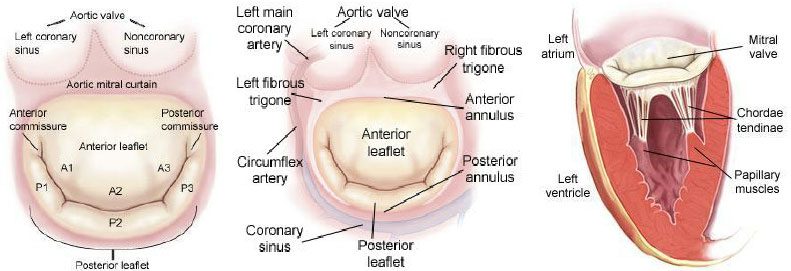
Mitral valve apparatus involves
- Two leaflets AML and PML
- MV annulus .
- Chordae tendinae
- Two papillary
Part of lt.ventricle
Pathophysiology of mitral stenosis
☛ Normal mitral valve orifice 4-6 cm2.
☛ Mild < 2.5cm2.
☛Mod 1.5 – 2.5 cm2.
☛Sev < 1 cm2
Rheumatic MS -valve leaflets thickening & fusion of commissaries → leaflet calcification & subvalval chordal fusion.
⤋
Mitral valve orifice reduces & limit diastolic flow in LV.
⤋
Fixed obstruction to LV inflow – Lt.atrial pressure rises progressively .
⤋
Limits pulmonary venous drainage and increases pulmonary capillary hydrostatic pressure when it goes more than oncotic pressure of blood pulmonary interstitial edema occurs with reflexly causes pulmonary arteriolar vasoconstriction & pulmonary artery hypertension.
⤋
Rt ventricular end diastolic volumes & pressure increases.
⤋
LA Enlargement
⤋
RV dysfunction → RV failure .
Is an almost unireversal finding in established mitral stenosis pateints. LA changes (1) Lt atrial dilatation (2) fibrosis of atrial wall (3) disorganisation of atrial muscle bundles → leads to disparate conduction velocities & inhomogeneous refractory period. Risk factor for development of atrial fibrillation.
Haemodyanamics in MS
Patient with MS tolerate tachycardia very poorly already there is fixed obstruction to LV inflow & tachycardia again reduces diastolic filling time so to maintain LV filling in a shorten diastolic pr. the flow rate across the stenosis valve increase. Because the valve area remains constant, the pressure gradient between Lt atrium & Lt ventricle increase by the square of the increase in flow rate according to Gorlins formula, in which mitral valve area calculated frm transvalvular pressure gradient and flow rate.
valve area= (transvalvular flow rate )/(2!constant × √Pg.)
Hydraulic consideration dictate that at given orifice size transvalular pr-gradient vs function of the square of transvalvular flow rate.
Thus doubling of flow rate causes – quadruples the pressure gradient.
Tachycardia necessitates a significant increase in the transvalvular pressure gradient & may precipitate feeling of breathlessness in awake patient.
- Mitral stenosis results in diminished preload reserve.
- LVEDV & LVEDP reduced with an accompanying decline in SV.
Causes of LV contractile impairment in MS
- Rheumatic myocarditis.
- Posterobasal regional wall motion abnormalities because of consequence of thickening & calcification of mitral apparatus.
- Vasoconstriction in response to low cardiac ant put may impair LV ejection.
- After load may also be increased due to inadequate myocardial wall thickness.
- Early RV filling displaces IVS to Lt side impairs LV
LV diastolic function impairment
Obvious impairment of LV diastolic filling as intrinsic compliance of Lt ventricle reduced by rheumatic disease process.
↑ transvalvular pr gradient – exercise, pregnancy, hyperthyroidism .All these conditions ↑ mitral valve flow – so transvalvular pressure gradiant increases hence it is very common to have 1st clinical manifestation in pregnancy.
Clinical features in MS
- with mild MS are asymptomatic same patient able to remain asymptomatic for long period by gradually reducing their level of activity in MS. (1.5cm2 – symptoms develop at rest.)
- with MS commonly report dyspnea as initial symptom – because of elevated LA pressure & pulmonary congestion.
- Palpitation – due to onset of atrial fibrillation.
- Systemic thrombi emobilisation occrue in 10-20%.
- Chest pain simulate angina may result from RV hypertrophy rather than Coronary artery disease.
Prognosis: depend on age of presentation of MS – 0-30 years in women.
☛ Now bcause of slow progression its presenting in 40-50s.
☛ After symptom develops MS remains a slow, progressive disease.
☛ Pt. live 10-20 years with mild symptoms such as dyspnoea with exercise.
☛ 10 years survival of Pt with mild symptom approaches 80% but 10years survival of Pt with severe disease without surgery is only 15%
At rest to produce cardiac output in critical ms <1 cm2 – Lt atrial pr. required 25 cm of Hg & transvalvular gradient required 20 mm of Hg.
Physical Examination Important pt. to remember
- Neck veins distended if Rt sided failure.
- Increase Rt Ventricular impulse in palpable along the sterna border.
- loud S1 at apex & narrow split S2 with accentuated P2 are audible if pulmonary artery hypertension present.
- Opening snap (short snapping sound accompaning the opening of mitral valve) may be audible in MS. OS Interval – 40-60 ms.
- Low pitch mitral diastolic murmur.-rumbling,best heard in lt.lateral position and holds breath in expn.,accentuated by exercise.
☛ ECG findings Rt axis deviation.
☛ Atrial Fibrillation.
☛ Lt atrial hypertrophy (LAH).
☛ Rt Ventricular Hypertrophy .
☛ X-ray findings 1) LA & RV enlarged main PA segment is usually prominent
- Lung fields show pulmonary venous congestions interstitial edam – kerley’s B lines.(dense, short horizontal lines in costophrenic angles) & redistribution of pulmonary blood flow with increased vascularity to upper lobes.
Causes of pulmonary venous hypertension in ms
- Passive due to backwards pressure of blood associated with elevated LA pressure
- Reactive due to pulmonary arteriolar constriction induced by PVH
- Organic Obliterative – permanent obliterative change in pulmonary vascular bed in response to clinically ↑ Pr in MS.
3 )Evidence of mitral valve calcification
4) Evidence of Lt.atrial emboli.
Management
Medical
- Mild & Mod Ms.- anticongestive measures (aggressive diuretics)
- Balloon dilatation of valve
- For AF – antiarrythemics, cardio version anticoagulation with warfarin should start 3 weeks prior to prevent systemic emobilisation of atrial thrombus & continue 4 weeks post cardiaoversion.
- Good dental hygiene & antibiotic prophylaxis against SBE.
- Restriction of activities
- Recurrence of rheumatic fever should prevent in children.
Surgical Decision making
Acc ACC/ASAguidelines indication area as follow
- Symptoms NYHA class III/IV MV gradient (dopplar)> 10mm of Hg
- Who are need careful assessment NYHA II/MV gradient > 10 ml teg need sx
- Sx is reasonable in pts with are asymptomatic but PA>50mm teg & mean MV gradiant >10m kg
- Failed balloon dilation or sev MR resulting from balloon dilation is an indication of sx
Surgical Procedures
☛ Closed or open commissurotomy for pliable noncalcified mitral valve.
☛ Mitral valve replacement
- MV – prosthetic valves – Starr – Edwards, Bjork – shiley, St – jude, Chitra valve.
- Require anticoagulation
- INR – 2.5 – 3.5
- With warfarin
- After biolorosthetic valve-Asprin 75 – 100 mg/day
Balloon Mitral Valvotomy
Goals
☛ ↑ effective mitral valve area
☛ Decreasing transvalvular pressure gradient
1st percutaneans mitral commissurotomy done by Inove in 1984
Technique directing balloon tip catheter across stenotic mitral valve.
Sequential inflation of distal & proximal portion ensuing correct positions across valve & inflating middle portion of device to split the fused commissures.
Most common complication – Mitral regurgitation .
MVR – prosthetic valves – Starr – Edwards, Bjark – shilay, St – jude, Chitra valve.
Require anticoagulation
☛ INR – 2.5 – 3.5
☛ With warferin
☛ After biolorosthetic valve 75 – 100 mg/day.
In detail Clinical aspect of MS in view of practical exam–
Symptomatology
- Haemoptosis
- Palpitations -AF
- Chest pain-RVH, low coronary perfection
- Fatigue – low cardiac output.
- embolic manifestations 50%
- Ortners syndrome – enlarged LA enlarged , tracheobronchial lymphnodes, dilated PA
Gives pressure on recurrent laryngeal nerve.
- Failure of RV – hepatomegaly, jaundice, anorexia, ascites .
- Infective endocarditis is common in mild MS than severe bcoz it occur in noncalcified thickened valve.
Five causes of haematosis
Wood suggested causes
- Sudden haemorrhage or pulmonary apoplexy
Rupture of thin walled bronchial veins in mild to mod MS
Sev. Long standing Ms they develop thick wale so haemorrhage slowly disappears with chroncity of NS
- Haemorrhage associated with paroxysmal nocturnal dyspnea
- Pink frothy sputum associated with pulm aedews ruptoe of alveolar capileces
- Blood tinged sputum associated with winter bronchitis chaic
- Haemorrhage associated with pulmonary infarction.
Causes of chest pain
- Dilated PA
- RV systolic overload due to PH co cause ischemia, producing pain
- Micro emobilisation of coronary arteries from calcified MS.
- Additional presence of CAD
Findings an X ray
- Lt atrial enlargement
- Straightening of left cardiac border.
- Double shadow on Rt side
- Widening of carnival angle
- Indention of oesophagusin barium
- E/O RV hypertrophy
- RV type of apex
- Lat X-ray shows RV occupying retrosternal space.
- E/O pulmonary hypertension
- Cephalisation – inverse moustache sign
- Upper lobe veins haling diameter of at less 3m
- Hasy lung field with kerloy ‘B’ line
- E/O pulm arterial hypertension
- Rt inferior decently an try of diameter 14m-25m
- Plemal effusion
- Signs of LA emboli
- presence of calcified emboli
- mitral calcification
Gen.Examination
☛ mitral facies pinkish – purple patches an check b/c low co & systemic vasoconstriction arterial pulse normal /feeble in Pt. With low C. O.
☛ Jugular venous pulse exhibits prominent ‘a’ ware palpable S1 – tapping S1 – AML is pliable.
☛ Lt lat recumbent position – apex Diastolic thrill of MS is palpable.
☛ Rt ventricle (enlarged) may displace Lt ventricle posteriorly.
☛ Loud pulmonic sound in Lt 2nd ICS due to pulmonary hypertension.
☛ Accentuated S1 with prolong Q- S1 interval
Opening Snap (OS)
Is caused by sudden tensing of valve leaflets after the valve cusps have complicated their opening excursion.
OS occur when the movement of mitral done into the left ventricle suddenly stops.
Most readily audible at apex using the diaphragm of stethoscope.
OS occur later than P2.
Mirral valve can’t be totally rigid if it produces on OS with is usually accompanied by an accentuated S1.
Calcification confined to tip of MV leaflets door no preclude OS
Short A2 OS interval reliable of sev. MS
Murmur – diastolic low pitched rumbling murmur apex with bell of stethoscope & with pt. In it lateral recumbent position.
Soft united to apex, when louder radiates to Lt axilla or lower Lt sternal border.
Duration of murmur – is guide to severity of mitral valve narrowing murmur commences immediately after OS.
Sev MS – murmur is low diastolic with presystolic accentuation achle SR maintained best heard pt lying in Lt Lat decubites position.
Dynamic auscultation -diastolic murmur & OS of MS reduced during inspiration & augmented during expiration.
Inspiration A2 – OS interval widens & 3 seqsandls A2, P2 & OS way be oudible sudden standing & resultant reductionof venous return lower the LA pr & widen A2 – OS interval but S2 Norrows on standing A2-OS Interval narrow on exercise.
Dialstolic rounmbing meause reduced during strain seven transmitavalve low rate declines.
Carey coombs murmur rhemartic mitral valvulitis ,soft early diastolic murmur.
Assesment of MITRAL valve- Echocardiography
Wilkins’s Score
|
Grade |
Mobility |
Thickening |
Calcification |
Subvalvular Thickness |
|
1 |
Highly Mobile valve with only leaflet tips restricted |
Leaflet near normal in thickness (4-5mm) | A single area of increased echo brightness | Minimal thickening just below the mitral leaflets |
|
2 |
Leaflet mid and base portion have normal mobility |
Mid-leaflets normal, considerable thickening of margin (5-8mm) | Scattered areas of brightness confined to leaflet margins | Thickening of chordal structure extending to ⅓ of the chordal length |
|
3 |
Valve continues to move forward in diastole, mainly from the base |
Thickening extending through the center leaflet (5-8mm) | Brightness extending into the mid-points of leaflets | Thickening extended to diastal third of the chord |
|
4 |
No or minimal forward movement of the leaflets in diastole |
Considerable thickening of all leaflet tissue (>8-10mm) | Extensive brightness throughout much of the leaflet tissue | Extensive thickening and shortning of all chordal structures extending down to papillary muscles |
Need of cardiac catheterisation – (1) Pts. Who have discrepancy between clinical& echo findings. (2) Pts with MS associated COPD to determine contribution of MS to symptoms. (3) Lt atrial my coma should be excluded (4) Pts. with angina pectoris (5) Men older than 40 years of age female >>0 years rule at CAD.
Anaesthetic considerations
☛ Anaesthetic considerations -Goals
☛ Preload – normal /↑ed
☛ After load – Normal.
☛ Rate – control ventricular response rate
☛ Avoid – Tachycardia, pulmonary vasoconstriction
- Avoidance of tachycardia in pre op period
To allay anxiety – small doses of narcotic or benzodiazepines
Aroid excessive sed’n may ↑ hypercarbia ↑ PVR and PAH so give O2 .
Maintain HR
Medicines – β- blocker, digitalis, calcium receptor antagonist .
- Ventricular rate control is primary goal in AF.
- hemodyanamic unstable AF – cardiovession can be done.
- Narcotic based anaesthetic induction is advisable to avoid tachycardia.
- Relaxant vecuronium, pancuronium can be given .
- Maintain of preload – judicious fluied management.
Invasive hemodynamic monitoring – arterial catheter and pulm art .catheter.
- Avoid ↑ PVR & ↑ PAH.