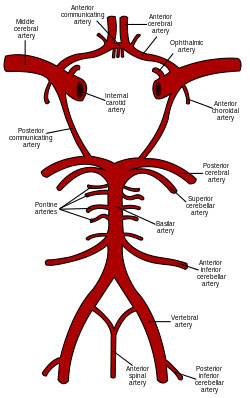
Circle of Willis
Common carotid origin
☛ Rt common carotid from Rt brachiocepholic trunk
☛ Lt common carotid from Arch of aorta
☛ In neck they travel in carotid sheath
☛ At level of thyroid cartilage they divide into external & internal carotid A.
☛ Internal carotid A passes through neck to enter middle cranial fossa without branching
Supplies
☛ hypophysis cerebri,orbit & major portion of supratentorial region.
☛ Cerebral arteries derived from ICA & vertebral arteries
☛ Two ant. cerebral arteries (braanch of ICA).
☛ Anteriorly forms circle of Willis with two ant. communicating Arteries.
☛ Two vertebral Arteries forms – basilar Artery which gives two post cerebral arteries which form posterior circle of Willis with two post. communicating arteries.
☛ Middle cerebral A supplies Lateral surface of each cerebral hemisphere
☛ Ant & post cerebral Arteries supplies medial & inferior surfaces of cerebral hemisphere
☛ Normal cerebral blood flow – 50ml/100ml/mm
☛ 4 time ↑ in gray matter then white water 80 & 20 ml/100gm/mm respectively.
☛ Metabolic requirement of oxygen in brain tissues 3 – 5 ml / 100gm/mm.
☛ Cerebral infarction depends on the degree & duration of ischemia.
Penumbra-neurons that are non-functional but that will recover fully with restoration of adequate flows are said to be penumbra
☛ If blood blow <10ml/100gm/mm- normal destruction occurs.
Cerebral auto regulation
☛ 50 to 150 mm of Hg
☛ If pr. above 150mofg vasoconstriction
☛ If pr. <50-vasodilation to maintain CBF in HTN patient limits are increased
☛Hypercarbia – cerebral vasodilation
☛Hypocarbia -vasoconstriction
☛Each mm Hg in PCO2 changes CBF 4%
Determinants
- Nerve call activity
- Cerebral perfusion pressure
- PaCO2
- pH
- PaO2
- neurogenic influences
Luxury perfusion blood flow in excess of metabolic need
Intracerebral steal response to hypercarbia decreases blood flow to ischemia area.
Inverse steal or Robin Hood syndrome
☛ Effect of hypocapnea vasocastriction ↑ blood flow to ischemic region of brain.
☛Vasoconstriction in adjacent normal arterioles causing local ↑in perfusion pr & augmenting collateral flow to ischemic,unreactive,maximally vasodilated area of brain.
CABG & Carotid Endarterectomy
- Combined lesion in one pt. If only CABG done 1st then 14% risk of stroke
- If only CEA done then 20% MI risk
Bernhard et al 1972 combined approach to carotid end arterectomy & CABG.
Frequency of stroke with cardiac sx 2 to 6%
CPB
- Embolic neurologic injury.
- An aortic cannulation.
- Plaque rupture duringg aortic cannulation.
- Release of aortic x clamp.
- Condiac manipulation according to transcraial Doppler USG.
Preop risk facters for stroke in pt undergoing CABG ON CPB.
- Carotid stenosis > 80%
- Carotid occlusion.
- Prior stroke or travsient ischemic attack.
- Peripheral vascular disease.
- Post infarction angina.
- Prolonged duration of CPB.
☛ Incidence of haemodyanamic significant carotid stenosis in pts needing CABG Varies between 2% & 16%
☛ Carotid bruit may be audible with minimal Carotid stenosis & silent with carotid lumen 1 -2 mm in diameter.
☛ USG with pulse Doppler & duplex scan are appropriate___ tests to assess need for carotid angiography – gold standared for evalution carotid stenosis.
☛ Hemipheic stroke – severe carotid disease can occure in CABG Pt with CPB.
☛ Stroke rate of combined operation is twice than each opevation alone.
☛ 5.5% stroke rate in unoperated carotid disease in CABG pt .
☛ 3.1% stroke rate who underwnt combined approach.
☛ Age > 70years have more stroke rate 40% carotid stenosis pts have CAD.
☛ Carotid Endarterectomy pt with severe symptomatic CAD has associated with 17% & 20% incidence of MI & mortality
No Myocardial Infarction in Combined approach CAD & CEA
- Shwarting et all – no difference in outcom when CEA was perfomed immediately before intiation of CPB or during hypo henic CPB
- Combined approach also decreasesa hospital stay & cost as well (Daily et all)
Anaesthetic considerations
Goals – maintain MAP without acceptable safe limit for brain as well as myocardial perfusion (middle to upper normal range without increases HR & after load)
- Normocapnia.
- Cerebral protection.
- Neuoro monitoring.
- Early extubation for neuro assessment outnight factors –hypothermia bleeding & haemodyananic instability.
aim for
- Protection of heart & brain
- Control of heart rate & BP
- ablation of sx pain & stress response
- Awake pt at the end of sx for purpose of neurological examination.
☛ Etiology of carotid endarterctomy
atherosclerosis.
☛ Symptons – attack of TIA amaurosis fugax – temporary Monocular blindness caused by TIA of retina .
☛ Risk of stroke – ↑ thrombosis, disruption of plaque .
Indication of Sx-
- TIA with angiographic evidance of stenosis.
- Reversibee ischemic neurologic deficit with >70% stenosis of vessel wall or an ulcerated plaque with / without stenosis.
- Unstable neurologic status persistant despite anticoagulation .
Pre-op evaluation-
- Freqent BP monitoring & target BP range should be decided.
- Continue all long term cardiac medications (aspirin 100).
- HTN
- DM -sugars level
- Investigations routine/specific.
Premedication mild sedation & anxiolysis intraop – monitoring-
- ECG – II, V5
- pulse oxemetry.
- intracrtrial pressure monitoring.
- if CVP require then – femoral or subclarian
GA
Goals
☛Induction mild midazolam, fentanyl , propofol + NDMR.
☛Esmolol/lignocain to obtend largyngoscopy reflex.
☛T/t of BP changes.
☛Pnenelepinephrene 50 to 100 microgram
☛Namisropruiside 6 to 25 us for st TN
☛Administration fluids, titration of anaesthetics & T/t of hypolension is very important.
☛Maintainance of anaesthesia – O2 + nitrous oxide 50%
☛isoflurane/sevoflurane
☛Haeneodyemanic fluctuations –
- Light plane
- Short acting vasocostrictors increases BP,
- ↑ HR/BP-↑myocardial ischemia
☛ Manipulation of carotid sinus – bradycavdia & hypotension
☛Infillrate carotid bifurcation with 1% lidocaine (may ↑ intra & postop HTN) .
☛End of Sx – titrate inhalations awaking – reversal of NMBA 4↑ or 100%
☛Place pt head up recumbent position/ quiten room.
Nemologic assessment
☛Period of emergence & Extubation associate with ↑ HTN & tachycardia tight hemodyanamic control is rewarding
☛Propofol group have less emergence crisis.
Regional & Local anaesthesia
- Blocking C2 & C4 – superficial & deep cerical plexus block.
- Local infillation of sx field – necessary sensing blockade.
Allows – 1. Continous neurolgic monitoring / assessment(most sensitive method to dectect cerebral ischemia)
- awoidance of expensne on neuromonitoring & ↓ vasopressor response and greater BP stability
- ↓ hospital stay & cost.
- Grater stability of BP
complications- loss of conciousness
seizures
- Disadvantage- pts claustrophobic anxiety, irritability,difficult neuromonitoring in uncooperative patients.
Relative contraindications
- Pt refusal for LA
- Difficult vascular anatomy
- Short neck, high biturcation, vigorous mandible retraction.
PH & glucose Monitoring-
- Cerebrovascular reactivity to CO2 is disturbed & autoregulatory capacity in ischaemic zone is lost.
Advisable – normocarbia
- M/o BSL below 200 mg/dl
Neurolgic M/M
- Stump pressure – <50 mm of Hg – hypoperfusion.
- Regional cerebral blood flow – injecting radioactive xenon.
- EEG – processed & unprocessed 16 lead per 7.5 to 20% pt EEG changes & influenced by contralateral stenosis leads to
- Shunt malfunction
- Hypotension
- Cerebral emboli
Limitation
- May not detect subcortical or small cortical infarcts.
- False negative results .
- Aftected by hypothermia, hypotention & anaesthetic depth.
- False positive result.
SSEP: based on response of sensory cortex to electrical impulscs from peripneral sensory nerve stimulation (sensory cortex – supplied by MCA at risk during carotid artery clamping).
So able to detect sensory pathway ischemia (CBF <12ml/100gm/min)
Tran cranial Doppler USG
Continuous measurement of mean blood flow Velocity & detection of micro embolic events in middle cerebral artery.
- 90% detection with TCD.
- Provide information regarding shunt function , embolic phenomenon.
- Post sx – emboli can detected by TCD
Infusion of dextran can ↓ incidence of emboli.
- Detects hyperperfusion syndrome
Cerebral oxygenation
- Jugular bulb venous monitoring.
- Continuous fibroptic jugular venous oximetry catheter available.
Near infra red spetrophotometry monitoring of reginal cerebral saturation through scalp & skull.
Postop
- Neurologic complication- emobilisation, hypo perfusion, cerebral hyper perfusion ,intra Cerebral haemorrhage.
- Hypertension – carotid sinus denervation.
- Cerebral hyper perfusion syndrome.
- Headache
- Seigure
- Focal neurologic signs.
- Brain edema
- ICH
- Hypotension – carotid body plays role.
- Cranial and cervical nerve injuries.
- unilateral recurrent laryngeal nerve palsy
- ipsilateral vocal card paralysis.
Carotid body denervation- Response to hypoxia , ventilary loss.
Wound haematoma .
dr.ajita.