Defination: The restoration of an adequate blood supply to a part of heart by means of a blood vessel graft [ aortocoronary bypass] or stenting the plaque site.
Anatomy of coronary arteries:
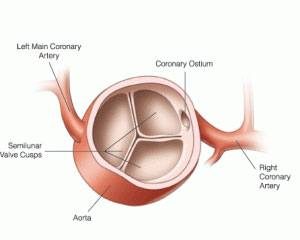
Aortic root-
Aortic root contains 3 cusps – Rt.coronary,Lt.coronary and non-coronary from first two cusps respective coronary arteries arises.

Coronary arterial circulation-
- Rt coronary artery
- Arises from Rt sinus of valsalva of aortic root.
- Best seen in Lt anterior oblique view 300 on angiography. (LAO 30°).
- Passes out straight for first few mm & then follows the Rt atrioveutricular groove & curves posteriorally within the groove to reach the crux of heart.
- Crux of heart:- Area where interventriclar septum meets AV groove.
- 85% RCA terminates as post descending artery (PDA) which is most imp. branch supplying posterior – superior IVS[interventricular septum].
- Gives branches to sinus node[65%], branch to AV node[85%].
- RCA said to be dominant when it crosses the crux of the heart & continues in the AV groove regardless of the origin of PDA (Anatomy) (Angiographers – dominant circulation depend on origin of PDA either from RCA Or Circumflex)
- Vertical & superior orientation of RCA from ostium allows easy passage of air bubbles during aortic cannulation, CPB or during open valve surgery. Perpendicular orientation of Left main coronary artery from ostium prevent air embolization .
- Lt Main coronary artery arises from Lt sinus of valsalva.
- Best seen in Rt. anterior oblique 10 o projection Lt main passes interiorly& to the left where it divides in a space between aorta & Pulmonary artery.
Branches are Lt anterior descending artery[ LAD] and Left Circumflex artery.
Left anterior descending artery-
☛ LAD passes anteriorly out of Interventricular groove it may reach only 2/3 of distance to apex or descend around the apex to the diaphragmatic surface.
☛ Branches of LAD -3 Diagonals
☛ Supplies to free wall of LV,
☛ septal branches courses posteriorly
☛ Supply portion of IVS
1st diagonal & 1st septal br. serve as imp landmark in description of lesions of LAD.
Left Circumflex artery
☛ Circemflex arises at sharp angle from the Lt main & courses toward crux of heart in AV groove.[ATRIOVENTRICULAR]
☛ When circumflex gives rise to PDA circulation is said to be Lt. dominant .
☛ Lt Coronary circulation supplies the entire IVS & AV node.
☛ 40% circumflex supplies SA node.
☛ Up tofour obtuse marginal arteries arise from the LCX & supply lateral wall of Lt Ventricle.
All epicardial branches give rise to small vessels that supply the outer third of myocardium & penetrating vessels that anastamose with subendo-cardial capillary plexus.
This capillary plexus unique in that it forms on end loop rather than anastomosing with an adjacent capillary from another epicardial artery .
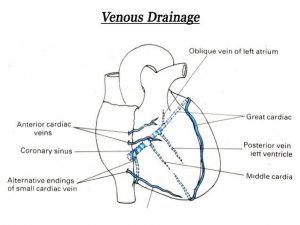
Venous drainage: → Coronary sinus which drains 96% of LV Free wall & septum. Reminder of the venous return goes directly to Rt. atrium small portion, two outer sinusoidal, ant luminal & thebesian vein.
Coronary artery disease-[CAD]
1 – Affect mostly pericardial vessels.
2 – Microcirculation disorders (+) even in normal coronary flow are present.
Atherosclerosis – most common at outer edges of vessel bifurcations blog in these region (i) blood flow slow & (II) changes during cardiac cyele resulting in net sheer stress which is less, (frictional force per unit) (III) low shcar stress stimulate atherogenic phenotype in endothelium.
Combined lesion of RCA & both branches of Lt Coronary artery termed as triple vessel disease.
Lt. Coronary artery supplies thickest portion of Lt ventricle, at least anterior two thirds of IVS & greater part of atria.
Coronary circulation
Peculiarities of Coronary Circulation:
☛ BF during diastole.
☛ End arteries.
☛ High capillary density.
☛ High 02 extraction.
☛ Regulation is mainly by metabolites.
☛ Anatomical anastomosis.
☛ The coronary vessels are susceptible to degeneration & atherosclerosis.
☛ There is evident regional distribution: The subendocardial layer in the left ventricle receives less blood, due to myocardial compression
(but this is normally compensated during diastole ).
However, this renders this area more liable to ischemia & infarction.
Myocardial ischemia & infarction: Myocardial perfusion depend on following two main factors- oxygen supply and demand.
| O2 Supply | O2 demand |
| O2 content of arterial blood | contractile state |
| Coronary blood flow | After load Preload Heart rate |
In patients with CAD[coronary artery disease] – myocardial ischemia usually results from imbalance between demand & supply.
Myocardial ischemia occur without changes in systemic haemodyanamics & in awake patients may occur in absence of chest pain. (silent ischemia).
Atherosclerosis is the most common cause of coronary artery disease.
Fundamental lesion is internal lipid plaque that causes chains stenosis & episodic thrombosis.
Characteristics of vulnerable plaque include high lipid content, thin fibrous cap, reduced no of smooth muscle cell & increase macrophage activity.
Lipid core is most thrombogenic component of the plaque.
Phase 1 small & progress very slowly.
Phase 2 high lipid content that has potential to rupture.
Phase 3&4 enlargement & fibroins tissue organization.
Phase 5 occlusive plaque.
Acute coronary syndrome (ACS) produced by sudden decrease in coronary blood flow.
unstable angina small fissure in plaque may produce temporary thrombotic occlusion of a vessel lasting 10 to 20 min.
Release of vasoactive substances from platelets & white blood cells as well as dysfunction of the endothelium may lead to vaso constriction & reduction of Coronary blood flow.
If occlusion lasts for 1minute – it produces non – Q wave MI.
While larger plaque discruption & prolonged thrombosis will produce Q wave infarction with transmural necrosis.
Coronary blood flow: independent of perfusion pressure but it is related to tissue O2 demand perhaps throbosis causes release a metabolite such as adenosine – this phenomenon is referred to as auto regulation.
All layers of ventricular wall maintaining essentially equal flows from epicedium to endocardium.
Difference between auto regulatory flow & maximal flow constitutes coronary vascular reserve.
As an obstruction of a coronary artery increases in size, dilation of the capillary bed occurs with maintenance of adequate blood supply as the result of reduced blood supply.
Coronary flow reserve however is diminished & eventually exhausted & auto regulation begins to fail.
Auto regulatory failure is loss of metabolic control of Coronary blood flow & the sole dependence on pressure gradients to determine flow.
Auto regulation fails first in subendocardium where blood flow fail to match demand resulting in subendocardial ischemia & dysfunction.
Auto regulation is pressure dependent, in that as perfusion pressure falls below a critical value auto regulation begins to fail.
Tachycardia ↑ O2 demand – ↓ diastolic time ↓ perfusion pressure – ↑ ischemia.
A coronary arterial stenosis may be rigid or more commonly 70% compliant in nature.
When the pressure in the coronary circulation distal to fixed stenosis is decreased, flow across the stenotic area decreases.
Clinical implication is that decreased blood pressure to an area of myocardium supplied by a vessel with a variable stenosis will decrease blood supply to the myocardium by two mechanism -1. loss of collateral flow and2. decreased flow across the compliant stenosis.
Collateral vessels exists in normal hearts best in presence of they are increase in size & number.
When a coronary vessel has a high grade stenosis the microvasculature distal to it may be maximally dilated even at rest & subject to ischemia.
Collaterals may develop between ischemia zone & an adjacent non ischaemic area supplied by a different vessel.
When vasodilatation of microcirculation is induced by exercise or drugs, perfusion of ischemic bed by collateral circulation may be decrease or cut off perticularly when the collateral vessels are poorly developed or it present at higher degree of resistance than collaterals that are well developed. when vasodilatation occurs in nonischamic area ,pressure within it is decreased,and flow across collaterals vessels with high resistance is reduced. Increase in myocardial blood flow in one region that reduces flow in another is referred to as coronary steal.
Hall mark symptom of myocardial ischemia is pain.
Myocardial revascularisation can be done by 1.Coronary artery bypass grafting
1.Percutaneous coronary artery stenting .
2.Coronary artery bypass grafting-aortocoronary grafts are prepared on coronary artery.
Arterial conduits are also used for grafting.e.g.Lt. and Rt.internal mammary artery,Radial artery.
Anaesthetic management is very crucial role in off pump bypass grafting surgeries.
Preop Evaluation & M/M
- Cardiac history & presenting symptoms.-status of cardiac function-NYHA
- Coronary artery anatomy.
- Ventricular function assessment.
- Valvalar & structural anatomy & function.
- Electrocavdiogram –
- Q waVe, ST-T changes
- Lt Bundle br block
Chest radiograph-
- cardiomegaly .
- Aortic calcification-difficult to top end grafting.atheroembolic episodes.
- Lung fields – Acute of chronic heart failure.
Assessment of Major Co- morbidities
- Carotid & cerebrovascular disease
- Peripheral vascular disease
- Diabetes Milletus
- Renal Disease
- Pulmonary disease
Preoperative medication management
- β adrenergic blockers
Recommended for all pts unless contraindication.
- calcium channel blocker
Higher incidence of heart block or need for pacing with β blocker therapy.
- ACE inhibitor
- Diuretics
- Statins
- Aspirin – should continue [institute protocol]
- Antiplatet agents or glycoprotein iia/iii b inhibitor associated with increased bleeding .
- Heparin
- Insulin – for control of ↑ BSL
- Oral hypoglycaemic agents – should stopped and insulin started.
- Antibiotic prophylaxis
- Anxiolytic or analgesic premedication
- Preoperative epidural insertion.
Intra-operative management
- IV access
- ECG
- BP monitoring – invasive arterial monitoring.
- Intra thecal medication – analgesia.
- Anaesthetic induction
- Muscle relaxation
- Maintain BP, HR, MAP
- ABGs
- ACT
- Foley’s catheter
- Temp monitoring
- Cerebral monitoring
- Pulmonary artery catheter
-
- Pharmacologic agents
Antifibrinolytic therapy
Steroids administered.
- Transesophageal echocardiography.
- Ryles tube
Coronary artery grafting can be done
- Off pump
- On pump.
[Details in CABG- seperate notes]
dr.ajita